Abstract
Introduction: Metformin may have anti-cancer properties through multiple mechanisms yet data are limited. In this study, we sought to examine the association between metformin use and the risk of incident hematologic and non-hematologic cancers.
Methods: We conducted a large retrospective cohort study among regular users of Veteran Administration (VA) care identified from the National Veteran Administration's clinical and administrative databases and Medicare. We included veterans aged ≥55 years with diabetes (DM) started on metformin or sulfonylurea (SU) between 2001-2012. We excluded patients with any prior cancer history (by ICD-9 code) or with missing data on kidney function, weight, race, and/or hemoglobin A1c. Drug exposure was assessed by extraction of medication lists from pharmacy databases (Clinical Data Warehouse and Central Management Server). Regular medication use was defined as filling ≥2 outpatient prescriptions per year. After initial prescriptions, a 2-year washout period was observed during which eligible patients continued regular use of initially prescribed DM drug, free of cancer, and had no exposure to other DM medications. Follow-up began at the end of the washout period and ended at first cancer diagnosis, death, oral DM medication change (metformin users started on/switched to SU and vice versa), or end of follow-up (July 10, 2016), whichever came first.
The primary outcome was any newly diagnosed cancer (≥2 ICD-9 diagnosis codes for the same cancer, ≥1 week apart, within 6 months). We further sub-categorized new cancer diagnoses as hematologic (leukemia, lymphoma, or multiple myeloma) and non-hematologic (solid tumors).
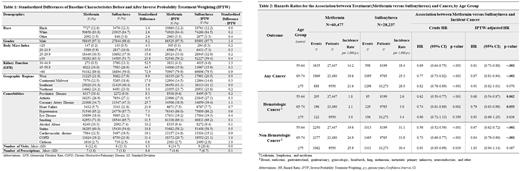
We used a new user design to mitigate risk of prevalent user bias and an active-comparator cohort of new users of SU to isolate metformin's effect beyond glycemic control. To minimize confounding by indication, we developed a propensity score and used inverse probability treatment weighting (IPTW). Baseline characteristics between metformin and SU groups were then compared to ensure similarity between groups. Cox proportional hazards models, using age as the time scale, were used to calculate hazard ratios (HR) and 95% confidence intervals (CI) for the association between metformin (vs. SU) and incident cancer.
Results: The study sample included 88,714 Veterans; mean age 68.6 ± 7.8 years; 98% male; 84% white, 13% black, and 3% other race. After IPTW, baseline characteristics were balanced between groups (Table 1).
We identified 60,477 metformin new users and 28,237 of SU new users. Over a mean follow-up of 4.2 ± 3.0 years, there were 7,383 incident cancer diagnoses, or 19.8 per 1,000 person-years (p-y); 17.5 per 1,000 p-y were in metformin users and 24.5 per 1,000 p-y were in SU users. Given the substantial effect modification of the association between medication use and cancer by age, a piecewise analysis was performed, stratifying the models by age group (55-64, 65-74, ≥75 years).
In patients 55-64 years, incidence of any cancer was 14.2 per 1000 p-y in metformin users and 18.4 per 1000 p-y in SU users. The association between metformin or SU and incident cancer had a crude HR 0.69 (95% CI 0.64-0.75) and an IPTW-adjusted HR 0.81 (95% CI 0.73-0.88). A similar trend was observed in patients 65-74 years: users of metformin had fewer incident cancers, with an IPTW-adjusted HR 0.87 (95% CI 0.81-0.94). However, in patients ≥75 years, cancer incidence did not differ between metformin and SU users, IPTW-adjusted HR 0.91 (95% CI 0.82-1.01).
Associations between metformin and incident hematologic cancers were similar to those observed for all incident cancers: in patients 55-64 years, IPTW-adjusted HR 0.68 (95% CI 0.54-0.87) and in patients 65-74 years, IPTW-adjusted HR 0.79 (95% CI 0.63-0.98). Incidence rates of hematologic malignancies in older adults (≥75 years) did not differ between metformin and SU groups (IPTW-adjusted HR 0.93 (95% CI 0.69-1.25).
Conclusions: Among U.S. Veterans with diabetes, new metformin users aged 55-75 years had lower incidence of hematologic and non-hematologic malignancies compared to SU users. Metformin use was not associated with cancer incidence among patients ≥75 years. Our findings make more urgent the need for randomized controlled trials to determine the potential of metformin in primary prevention of cancer in both solid and liquid tumors, as well as further studies into the mechanism of metformin's anti-cancer effects.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.